Nursing Care Plan for Heart Failure
Overview
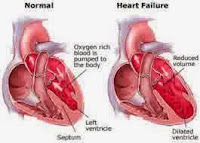
Heart failure is a chronic condition where the heart cannot pump blood efficiently, leading to insufficient oxygen delivery to the body's tissues. This debilitating condition affects millions worldwide and can result from various causes, including coronary artery disease, hypertension, and myocardial infarction.
Symptoms of heart failure include shortness of breath, fatigue, swollen ankles, and a reduced ability to exercise. It significantly impacts a person's quality of life and requires comprehensive management strategies involving lifestyle modifications, medications, and, in severe cases, surgical interventions such as heart transplantation.
Understanding the risk factors, recognizing symptoms, and seeking timely medical intervention are crucial aspects of managing heart failure. With the advancement of medical research and technology, treatment options continue to evolve, offering hope for improved outcomes and enhanced quality of life for individuals living with heart failure.
NOC:
- Cardiac Pump effectiveness
- Circulation Status
- Vital Sign Status
- Vital Signs in the normal range (blood pressure, pulse, respiration).
- Can tolerate the activity, there is no fatigue.
- There are no pulmonary edema, peripheral, and no ascites.
- There is no loss of consciousness.
NIC:
Cardiac Care
- Evaluation of chest pain (intensity, location, duration).
- Note the presence of cardiac dysrhythmias.
- Note the presence of signs and symptoms of cardiac putput decline.
- Monitor cardiovascular status.
- Monitor respiratory status that indicates heart failure.
- Monitor the abdomen as an indicator of decreased perfusion.
- Monitor fluid balance.
- Monitor any changes in blood pressure.
- Monitor the patient's response to the effects of antiarrhythmic treatment.
- Set the period of exercise and rest to avoid fatigue.
- Monitor the patient's exercise tolerance.
- Monitor the presence of dyspnea, fatigue, tekipneu and ortopneu.
- Suggest to reduce stress.
Vital Sign Monitoring
- Monitor BP, pulse, temperature, and respiration.
- Note the presence of fluctuations in blood pressure.
- Monitor vital signs while the patient is lying down, sitting, or standing.
- Auscultation BP in both arms and compare.
- Monitor BP, pulse, respiration, before, during, and after activity.
- Monitor the quality of the pulse.
- Monitor the presence of pulsus paradoxus.
- Monitor the presence of pulsus alterans.
- Monitor the amount and heart rhythm.
- Monitor heart sounds.
- Monitor the frequency and rhythm of breathing.
- Monitor lung sounds.
- Monitor abnormal breathing pattern.
- Monitor temperature, color, and moisture.
- Monitor peripheral cyanosis.
- Monitor the presence of Cushing's triad (widened pulse pressure, bradycardia, increased systolic).
- Identify the cause of the vital sign changes.
Bibliography:
1. Ponikowski, P., Voors, A. A., Anker, S. D., Bueno, H., Cleland, J. G., Coats, A. J., ... & ESC Scientific Document Group. (2016). 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European Journal of Heart Failure, 18(8), 891-975. doi:10.1002/ejhf.592
2. Yancy, C. W., Jessup, M., Bozkurt, B., Butler, J., Casey, D. E., Colvin, M. M., ... & Wilkoff, B. L. (2017). 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Journal of the American College of Cardiology, 70(6), 776-803. doi:10.1016/j.jacc.2017.04.025